Takeaways from Moving With MS Support Group:
hosted by MS Views & News, presented by
Dr. Gretchen Hawley PT, DPT, MSCS
December 2023:
Our topic tonight was Pain & Sensory Changes in MS!
A few helpful links that were shared:
1. Exercises to reduce MS Spasticity - this is relevant if you feel your pain is caused by tight/spastic muscles.
2. Places to find an MS-specialized physical therapist who can hopefully help you differentiate pain related to orthopedic reasons vs. MS:
- National MS Society Care Partner Program
- Consortium of Multiple Sclerosis Centers
- American Physical Therapy Association "Find a PT"
3.Here is the YouTube page you can go to to watch our past Moving w/ MS Virtual Support Group webinars: https://bit.ly/3oCyhYG
August 2023:
Here are the links we reviewed that show examples of modifications and exercises you can do throughout the day:
→ Modifications:
https://www.instagram.com/reel/CL76K8pjuO1/
→ Exercise throughout the day:
https://www.instagram.com/reel/CUGpns8DG6T/
https://www.instagram.com/reel/CThqesFDDN_/
https://www.instagram.com/reel/CQgqEbXDTp9/
https://www.instagram.com/reel/CUsYmh1jGgW/
https://www.instagram.com/reel/COddRoyDOqf/
https://www.instagram.com/reel/CKuBH6_DZkk/
https://www.instagram.com/reel/CIoE0gYDOcl/
https://www.instagram.com/reel/CKNdwutjfyo/
→ Here is the YouTube page you can go to to watch our past Moving w/ MS Virtual Support Group webinars: https://bit.ly/3oCyhYG
July 2023:
Here is a list of helpful links we discussed in the webinar on helpful tools, aids, and devices!
June 2023: Strength vs. Endurance Training for MS:
Here are some helpful links that were shared on the support group call:
1. Dr. Grip Pen - beneficial for those that have difficulty holding onto a pen
2. YouTube Channel for Arthritis Life - Occupational Therapist that shares helpful tools for those with hand weakness/aches/pains
3. YouTube Channel for Equip Me OT- Occupational Therapist that shares helpful tools for those with limited mobility or looking to save energy
4. YouTube video for stiff & achey joints (from Dr. Gretchen's youtube page)
5. If you're not already on my Book Launch Waitlist, sign up HERE. You'll stay up to date with the book launch, get sneak peeks into the book, get VIP early access, and extra bonuses if you purchase the book during launch week (like a free pdf of all the exercises in the book!!!)
November 2022: How To Modify An Exercise Routine
1. This is the recording of the MS-specific walking webinar to help improve walking and reduce leg swing/circumduction.
2. To access past recordings of our Moving with MS support group, including functional exercise, click here.
October 2022: Functional Outcome Measures
1. Modified Fatigue Impact Scale: https://www.sralab.org/sites/default/files/2017-06/mfis.pdf
2. Multiple Sclerosis Walking Scale-12: https://www.sralab.org/sites/default/files/2017-07/msws-eng.pdf
3. Dynamic Gait Index: https://arborrehab.com/images/uploads/general/Dynamic_Gait_Index.pdf
4. The MSing Link app (with instructional videos explaining functional outcome measures + a place to track each one):
> Download the app for Android
> Download the app for iOS
5. Link to watch recordings of our Moving w/ MS Virtual Support Group: https://bit.ly/3oCyhYG
8/8/22: Bad Habits
-
Putting a lot of weight through your mobility aid / slouching
- Instead... practice putting less weight through your upper body when walking + strengthen & stretch appropriate muscle groups!
-
Touching walls/furniture/humans
- Instead... practice walking without touching walls. Stay close to the wall, at first, then work your way to walking in the middle of a room. If too challenging, use a mobility aid!
-
Using your arms to lift your leg
- Instead... use your hip flexors instead! Strengthen them via seated marching!
6/27/22: Assistive Device Q&A
Here are a few products that were mentioned during the show & tell/discussion about helpful mobility aids:
Crutcheze - to hold up your cane
6/7/22: Assistive Devices/Mobility Aids
There were a few links being passed around during the meeting. You can find them below:
2. Rollz Rollator/Wheelchair Duo
3. Naboso Toe Splays -can help with toe curling while standing/walking; Use code DRGRETCHEN for 20% off (I do not receive commission or credits).
4. My Foot Shop - Crest Pads can help with toe curling while standing/walking.
5. Recordings of Moving with MS webinars!
6. My YouTube Video on AFOs
7. My YouTube Video on MS specific balance/walking with or without a mobility aid!
1/10/22: Spasticity
1. Modified Ashworth Scale is used to asses your level of spasticity: 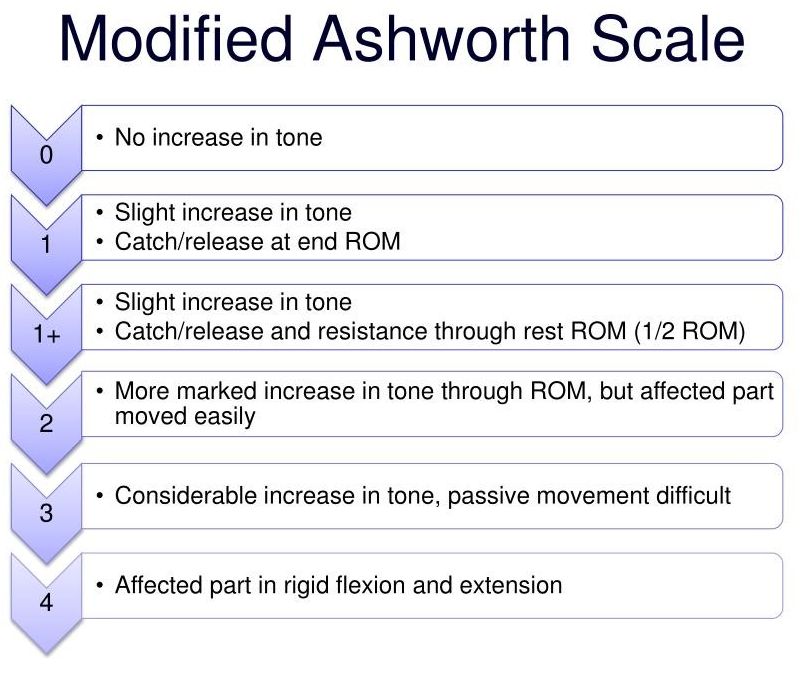
2. Treatment for spasticity:
- Physical Therapy + Occupational Therapy
- passive stretching
- splints/casts
- Medications
- Baclofen, Tizanidine, Diazepam,
- Botulinum Toxin/Botox injection
- Surgery
- Intrathecal Baclofen Pump
- Rhizotomy: cuts away part of the spinal nerve
- Tenotomy: tendon release
3. Types of stretching:
- Active - on your own
- Passive - assisted (by someone else)
- Static - longer holds; 20-30 seconds, 2-4x/side
- Dynamic - shorter holds; 2-3 seconds, 20-30 repetitions
- PNF stretching - on an angle, w/ resistance
4. Clonus = a bouncing of the leg due to the angle of your ankle. The more flexed your ankle is, the more your ankle will "bounce", causing your leg to bounce. It relates to lesions in the upper motor neurons. To reduce clonus, straighten your leg and point your toes away from you.
12/20/202: Scheduling Your Day
1. Start with making a list of your goals/outcomes for the week.
2. Then make a list of your necessities (ie: breakfast, lunch, dinner, medication, shower, etc.)
3. Then break down your goals into many smaller tasks. For example, if you have a goal to complete writing holiday cards by the end of the week... you can delegate 1 hour for 4 days to write cards. Or, if you plan on exercising at a gym... you can break that down to a) getting dressed for the gym, b) driving to the gym, c) exercising, d) driving back home
4. Once you have all of your goals broken down... go ahead and schedule them in Google Calendar (or any system you like; pen & papper works well, too!)
5. Make sure to plan for extra time for each task. Also, leave blank slots throughout your day to ensure you don't expend too much energy. Lastly, it's smart to create a "back up" time in case you weren't able to do your exercise earlier in the day.
6. To view the playlist/recordings of our 2021 Moving w/ MS Support Groups, click HERE!
11/8/2021: CMSC Research Updates, Part 1
1. To promote remyelination, we need:
- Stimulate OPCs - Drugs that have been found to do this in mice = benztropine, clemastine, clobetasol, miconazole, metformin
- Mobilize OPCs → through exercise!! Exercise increases oligiodendrogenesis after demyelination. Also, exercise promotes remyelination (shown this on a cellular level).
- Improve the lesion microenvironment- by Reducing CSPGs (Fluorosamine & difluroosamine). Difluorosamine has also shown increase in OCPs.
- Modulate inflammation/microglia activity (possibly through Niacin?)
2. High Dose Biotin not found to be effective for MS.
3. Wahls Protocol & Swank Protocol equally effective to improve cognition, motor function, and fatige.
4. Cannabis may be effective in treating spasticity. More research is needed.
- THC: psychoactive component, can help with nausea & vomiting
- CBD: can help with neuropathic pain
- Other medication interventions: Sativex (THC + CBD) - approved in Canada & Europe for MS symptoms including spasticity & pain
- Ketamine: being used for acute and chronic pain as well as mood disorders
5. BTK Inhibitors = a new DMT in clinical trial that can enter the brain and spinal cord. Also may be able to promote repair + reduce inflammation to allow for remyelination.
10/4/2021: Motivation & Consistency
1. Pick one exercise & start small. Just do one set of as many as you can with good quality!
2. Pick a time of day that works for you!
3. Think positive thoughts before, during, and after your exercise(s).
4. Create your "why statement". Ask yourself why you want to stay consistent with exercise... what will it result in? Then keep asking yourself why until you have an answer that evokes emotion.
5. Remind yourself of your positive proof of why this IS possible for you! What things have you accomplished in the past that you stuck to? This is proof that you CAN stick to your exercise program because you've been consistent with things in the past.
6. Surround yourself with positive success stories. This can be anything online (social media accounts, youtube videos, blogs) or audiobooks, paperback books, journals, etc. Get an accountability partner or an accountability group! This support group is a great first step!
★ To learn more about my live Zoom exercise classes, click here.
9/14/2021: Functional Exercise
1. In order to pick which exercises to do… pick an activity that is challenging (that you’re hoping will get easier), and break that activity down into many different movements. Those movements should be your exercises.
2. The number of repetitions and sets is different for everyone. Shoot for 30 perfect (or close to perfect) repetitions, taking as many rest breaks as you need to.
3. “General” exercise is good for general strengthening and cardio, however it often doesn’t translate to making movement easier. For example, having full strength in an exercise on the floor (i.e. clamshell exercise) does not mean that your walking will be easier/stronger/more stable.
4. Functional exercise means you exercise in the same (or similar) position of the movement you’re working on. For example, if you’re working on improving your walking… you’d benefit from standing exercises and sitting exercises… not exercises laying on the floor.
5. Helpful links:
Leg Lifter
Car Cane
7/12/2021: Strength vs. Endurance
1. Use this link to find an MS PT from the MS society
2. Seven steps of walking = weight shifting, bending your knee & straightening your knee, lift your ankle, lift your knee/hip, heel placement, single leg stance
3. Strength definition =
- Muscle gain to perform a movement
- The amount of force you can put out or the amount of weight you can lift
4. Endurance definition =
- Muscle gain to SUSTAIN a movement
- How many times you can do a movement without fatiguing
5. For endurance, push to the point of fatigue, but stop as soon as you feel fatigued. You should never exercise through bad form
6. Examples:
Holding a mug
- Strength: grasp the mug
- Endurance: continue holding the mug
Brushing our hair
- Strength: grasp the brush + lift your arm
- Endurance: continue holding your arm up
Walking
- Strength: lift your legs
- Endurance: walking for 5 minutes, instead of 1
6/7/2021: MS-Specific Physical Therapy
1. Orthopedic physical therapists tend to focus on general strengthening exercises, whereas an MS Specialized PT focuses on functional exercises that will help improve function (not just strength).
2. MS Certified Specialists must have observation hours of a PT working with someone who has MS + treatment hours with people who have MS + passing the MSCS exam. Additionally, they're required to attend continuing education to stay on top of MS resources and treatment.
Neuro Certified Specialists (NCS) have more education on neuro-based diseases than orthopedic physical therapists and are a good backup option if you don't have an MS-specialized PT in your area.
3. Physical Therapy can help with:
- Strength
- Balance
- Flexibility
- Aerobic Endurance
- Spasticity
- Fatigue
- Depression
- Walking Performance
- Quality of Life
...even with a progressive disease like MS!
4. An MS Specialized PT should always take your fatigue & heat intolerance into consideration. You should stop an exercise prior to fatigue, take breaks, and stay cool during your PT session.
5. Where to find access to an MS-Specialized PT:
1. In-person PT
* Search your local MS Society Care Partners
* Contact Consortium of MS Centers
* Call local PT clinics
2. Telehealth PT
3. Online MS Exercise programs (we discussed The MSing Link
6. To find a Pelvic Floor PT, try: https://pelvicguru.com
5/10/2021: Assistive Devices
1. When you should consider using a mobility aid:
- If you’re a “wall walker” or “furniture walker”
- If you feel unsteady
- Increased frequency drop foot or “foot catch”
- If you have falls - controlled or not
- If you have “almost-falls”
2. Consider the base of support (BOS)/width of the bottom of the device. Trekking poles have a very small BOS, meaning it isn't as stable as a cane, which has a wider BOS. Similarly, a walker or rollator has 4 legs with a wide BOS, so a walker/rollator will feel more stable than a cane.
3. Taller assistive devices typically will not improve your posture. Typically, you'll still have a slouched position but your arms will be higher. In order to improve posture while walking with a mobility aid, you need to focus on strengthening/stretching exercises for your back and hips.
4. How to fit a mobility aid to your body:
- Stand up tall & place arms down by your side
- Adjust the height of the handle to be in line with your wrist bones
- Try it out!
5. If/when using a cane, make sure you use the cane on the opposite side of the weak leg. Additionally, place no more than 50% body weight through the cane to prevent slipping and reduce likelihood of arm pain.
4/5/2021: Spasticity & Stretching
1. Muscle Spasm: When a muscle involuntarily contracts, then relaxes.
Muscle Cramp: same as spasm, but lasts longer.
Spasticity: muscles stiffen/tighten, preventing normal fluid movement
* can affect movement, gait, speech, etc.
* imbalance of electrical signals from the brain and spinal cord
2. Treatment for muscle tightness/spasm/cramp:
- Muscle stretching
- Stay hydrated
- Exercise/move regularly
- Improve nutrition: magnesium, protein
- Muscle relaxers: Capsaicin, Arnica, Icy Hot, Tiger Balm
3. Treatment for spasticity:
- Physical Therapy + Occupational Therapy
- passive stretching
- splints/casts
- Medications
- Baclofen, Tizanidine, Diazepam,
- Botulinum Toxin/Botox injection
- Surgery
- Intrathecal Baclofen Pump
- Rhizotomy: cuts away part of the spinal nerve
- Tenotomy: tendon release
4. Types of stretching:
- Active - on your own
- Passive - assisted (by someone else)
- Static - longer holds; 20-30 seconds, 2-4x/side
- Dynamic - shorter holds; 2-3 seconds, 20-30 repetitions
- PNF stretching - on an angle, w/ resistance
5. Newer research shows prolonged static stretch can be helpful for spasticity, indicating holding a stretch for up to several minutes long.
3/22/2021: General Symptom Management Q&A
1. Many people asked about the workshop I co-hosted with Mindy Eisenberg re: adaptive physical therapy and yoga. We reviewed principles of adaptive PT and yoga and demonstrated many exercises & poses. You can watch the recording HERE!
2. The MS Hug can be a symptom of Multiple Sclerosis. This is often described as a sensation of tightness around your chest/abdomen. Some things you can try to reduce this sensation are:
- Stretching of your torso
- Movement of your upper body (ie: yoga, pilates, light arm exercises, etc.)
- Medication (ask your doctor about a short dose of corticosteroids or any other drug that may help)
3. We discussed the Dictus Band for foot drop. This is an ankle strap with an elastic band that assists with lifting your toes up to prevent or lessen foot drop. Please note that this is NOT effective if you have no strength in your ankle (ie: if you can't lift your toes up the ground at all) however it is very effective if you have some strength in the ankle. You can find it HERE.
4. We talked a lot about the various symptoms that can arise due to heat intolerance. Best strategies to reduce heat intolerance are:
- Sip ice cold water
- Wear a cooling device (my favorite cooling vest is the Thermapparel Cooling Vest and I also love the Hyperkewl Cooling Wrist Bands)
- Take breaks if you're exercising or moving around (ie. chores, errands)
*Remember that heat intolerance can kick in on a hot day even if you're indoor in air conditioning! Similarly, it can kick in during the winter if you're bundled up in lots of clothing layers.
3/8/2021: General Symptom Management
1. Heat Intolerance is when your core temperature rises by at least 1/2 of a degree, causing one of several symptoms to worsen. Cold Intolerance is when your core temperature drops by at least 1/2 of a degree, causing one of several symptoms to worsen. Heat/Cold Intolerance can be caused from anything that causes core temperature change: outdoor temperature, showers, exercise, stress, etc.
2. Peripheral Vertigo (most commonly, BPPV) and Central Vertigo (caused by MS) can both occur in people with MS. The treatment = treat the cause. For BPPV, the treatment is typically the Epley maneuver. For Central Vertigo, the treatment is typically anti-motion-sickness drugs or a short course of corticosteroids. Talk to your doctor about best treatment for you.
3. One of many cognitive challenges with MS is difficulty doing 2 things at once, ie: walking and having a conversation. You can train this by practicing doing two things at once. For example, practice counting backwards from 100 by 2's while doing the marching exercise.
4. Overactive/Spastic Bladder is a common symptom in MS. This can look like: urinary frequency, urinary urgency, hesitancy, incontinence, difficulty emptying, etc. Treatments can include:
- Diet modifications
- Adequate fluid intake
- Bladder training or planned voiding
- Medications
- Pelvic Floor Physical Therapy
- Percutaneous Tibial Nerve Stimulation
- Intermittent Self-Cathetertization
- Surgical Interventions
5. The most common bowel symptom is constipation, however diarrhea can also be a symptom of MS. These are typically caused from reduced sensation, muscle weakness, increased tone, fatigue, reduced mobility, etc. Best treatments typically include:
- Getting physical activity
- Drinking adequate amounts of fluid
- Include plenty of fiber in your diet
- Establish a regular time & schedule for emptying the bowels (bowel training/retraining)
- Medications: ask your doctor
These interventions may take several weeks to know if they're working, so be consistent and patient.
2/23/2021: Q&A re: Sensory Changes
1. Sensory changes can sometimes be caused from tight muscles. If this is the case, stretching those muscles can help loosen the tension on the nerve and therefore reduce sensory changes.
2. CBD oil has been an an effective strategy (anecdotally) to reduce sensory changes. Make sure you are diligent in finding good quality CBD from a reliable source.
3. If your sensory symptoms are brought on by something that you touch, desensitization strategies may be helpful to reduce the sensations. These exercises/strategies may be less helpful if your sensory issues are not brought on by any specific thing you do.
4. You can find information on my online MS wellness program, The MSing Link, here. You can sign up for my live exercise classes here. The site will require you make an account in order to sign up for a class.
2/8/2021: Sensory Changes - Numbness, Tingling, Pins & Needles and more
1. Why do these sensory changes occur? Demyelination causes changes to the sensory portion of our nerves. Our brain can’t interpret a specific sensation, so it tries to relate it to something you’ve already felt or KNOW how it feels (ie: tingling, pins & needles, numbness, etc.)
2. There is no actual damage to the part of your body that you’re feeling the sensory change… the damage is in the nerve that reports to the brain from that area.
3. Treatments include:
Medications
- Botox
- Pulsed Magnetic Field
- Baclofen
- Gabapentin
- Antidepressants
- Others
Therapies
- Occupational Therapy
- Physical Therapy
- Exercise
- Massage
- Heat/Cold Packs
- Others
4. Knowing your TRIGGERS for sensory changes can be very helpful in reducing the severity of the sensory change(s).
Potential triggers: heat, cold, stress, exercise, sexual issues, things you use (pen, cup, fork, etc.), chair you sit in, etc.
5. Desensitization exercises include using materials (cotton ball, fabric, comb, pen, etc.) or sensory objects (rice, dried beans, marshmallows) over the area that has sensory changes. The idea is to provoke the sensory change and get your skin used to that feeling. Eventually, it shouldn't bother you as much since it is a de-sensitization strategy.
1/25/2021: Q&A from Strengthening & Functional Exercise
1. In order to improve your standing position, you first need to determine which is the bigger issue: a weak back (aka: rounded back) or weak hips (back is flat, but hips are sticking outward). If the issue is your back, you can stretch your pecs & strengthen your back muscles. If the issue is your hips, you can stretch your hip flexors & strengthen the glutes, hamstrings, etc.
2. To improve foot drop, it's best to stretch the calf and strengthen the front of the ankle.
3. Marching is one of my favorite functional exercises that can help with walking, stair climbing, scooting in your chair, getting into and out of a car, getting into and out of your bed, etc.
4. The muscles that cause knee buckling and/or knee hyperextension are your quadriceps muscles. Strengthening these muscles should help reduce knee buckling and knee hyperextension.
5. If you don't walk, there are many seated exercises you can do to improve strength in your arms, core, and legs. This strength will help with transfers, posture, and so much more. Don't give up!
* We discussed my Free 5 Day MS Strength Challenge - you can learn about it HERE. We start Monday February 1st.
1/4/2021: Strengthening & Functional Exercise
1. In order to pick which exercises to do… pick an activity that is challenging (that you’re hoping will get easier), and break that activity down into many different movements. Those movements should be your exercises.
2. The number of repetitions and sets is different for everyone. Shoot for 30 perfect (or close to perfect) repetitions, taking as many rest breaks as you need to.
3. “General” exercise is good for general strengthening and cardio, however it often doesn’t translate to making movement easier. For example, having full strength in an exercise on the floor (i.e. clamshell exercise) does not mean that your walking will be easier/stronger/more stable.
4. Functional exercise means you exercise in the same (or similar) position of the movement you’re working on. For example, if you’re working on improving your walking… you’d benefit from standing exercises and sitting exercises… not exercises laying on the floor.
5. The recumbent bicycle is good for general strengthening & cardio, but it does not help with walking due to the fact that your muscles are working in a reclined seated position vs. standing.
Thank you to our supporters:


Want to continue learning?
Check out some of these resources:

